
How to write
SBAR Nursing Example: How to Communicate Patient Information Clearly
Author: Michael Perkins
Updated: Jul 22, 2025
min
Table of contents
The SBAR example nursing tool is a successful method of organizing and sharing patient information. It’s an acronym for Situation, Background, Assessment, and Recommendation, which helps with clear and quick communication.
This guide breaks down the SBAR meaning and shares practical SBAR examples for nursing students who want to get more confident in clinical settings.
And, if you need help writing any nursing assignment, professional essay writers are here with expert support to make it easier.
What Is SBAR in Nursing?
SBAR is a structured way for nurses to communicate patient information with a healthcare provider (HCP) or other nurses. It stands for Situation, Background, Assessment, Recommendation. This focused communication method guides nurses to give relevant information only so that the care team acts quickly and effectively, especially when even seconds count.
It actually started in the U.S. Navy to improve fast, high-stakes communication and later found its way into hospitals. Now, it’s one of the most trusted tools in nursing for making sure everyone on the care team is on the same page.
In nursing, SBAR supports:
- Verbal communication with doctors and other healthcare professionals
- Written communication tools like reports or patient handoffs
- Documentation for clarity in medical records
- Patient care discussions within the healthcare team
The Importance of Using SBAR in Nursing
SBAR is a great communication tool and is especially useful when things are moving fast. It helps the healthcare team understand the patient’s condition and stay on the same page. Here’s how SBAR makes a difference in daily nursing work:
- Improves patient safety by cutting down on mixed messages during handoffs.
- Helps the team make faster, more informed decisions with the right details upfront.
- Makes it easier for nurses to share key updates without second-guessing what to say.
- Keeps everyone aligned by using a shared communication structure across the unit.
- Prevents mistakes by filtering out unnecessary information and highlighting what’s important.
How to Write an SBAR?
Writing an SBAR is about getting straight to the point without missing what matters. Start by explaining the patient’s current situation. Then share a bit of background to help make sense of it. Describe what you’ve noticed or are concerned about, and suggest what needs to happen next. Follow the detailed SBAR report example below:
S = Situation
This is where you explain what’s happening right now. You quickly communicate the patient’s current issue and let the team know why you’re reaching out.
Example: ‘This is Jane from Med-Surg, calling about Mr. Lee in room 204. He’s experiencing new-onset chest pain.’
B = Background
Here, you share a relevant background that helps explain the situation. Keep it brief but useful. This can include the following in your SBAR documentation example:
- Admission date
- Allergies, IV fluids running, medication
- Client’s code status
- Consults
- Admitting diagnosis
- Recent procedures
- Vital signs trends
- Medications
Example: 'He was admitted yesterday with a diagnosis of coronary artery disease. His last vitals were stable, but now his blood pressure is elevated, and he's complaining of pressure in his chest.'
A = Assessment
In this part, you describe what you think is going on. This is based on what you’ve seen, heard, or measured.
Example: 'His chest pain began suddenly and radiated to his left arm. He looks pale and his pulse is irregular.'
R = Recommendation
This is where you suggest what should happen next. Make it clear and specific.
Example: 'I recommend doing a formal chest X-ray and notifying the on-call physician for further evaluation.'
Recommended article: Research paper outline template
How to Use SBAR in Communication?
SBAR is a tool designed to make your job easier and to communicate important information without second-guessing yourself. Here's how to use it in real conversations:
- Start with the Situation: Say who you are, who the patient is, and what’s happening right now. Keep it short and specific.
- Give the Background: Share the important details that help explain the situation. Think diagnosis, admission date, recent vitals, meds, or anything that’s changed.
- Share Your Assessment: What’s your take on what’s going on? Mention what you’ve seen, heard, or measured. Stick to facts in your nurse SBAR example.
Also worth reading: AI vs Human Writing
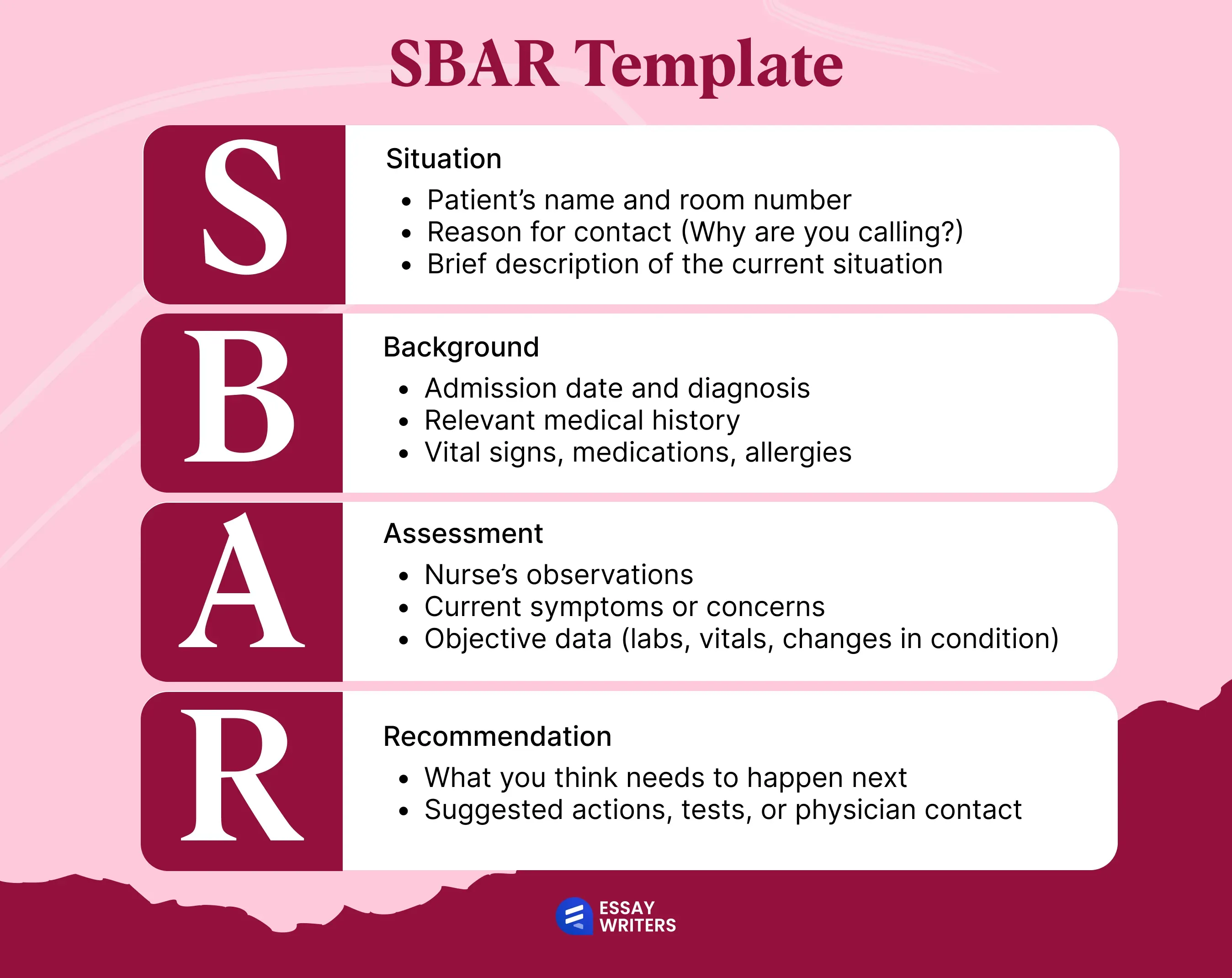
SBAR Template for Nursing Students
If you're new to SBAR, this template will help you clearly structure your work, stay focused, avoid rumbling, and not leave anything important. Great for clinicals, sim labs, or just getting more confident with your reports.
Nursing SBAR examples are great, but if you're still unsure how to structure your assignment, our essay writers offer personalized help with nursing assignments.
Templates are great, but if you're still unsure how to structure your assignment, our essay writers offer personalized help with nursing assignments.
SBAR Nursing Example
Knowing the structure of SBAR is one thing; actually using it in real situations is another. Having a go-to framework helps keep your message clear, focused, and helpful, whether you’re talking to an on-call HCP or giving handoff to another nurse. Below are five practical SBAR nursing examples based on situations nurses face often. Each SBAR communication example shows how to use this method to relay patient information effectively.
If you need extra support mastering clinical writing, our graduate essay writing service is here to help with SBAR reports, care plans, and other nursing assignments.
Example №1: Chest Pain in an Older Adult
- S: This is Sarah, RN on Med-Surg. I’m calling about Mr. Jackson in room 312. He’s reporting new chest pain rated 7 out of 10.
- B: He was admitted two days ago with a diagnosis of congestive heart failure. His last vitals were stable, but now his blood pressure is 170/96, and his pulse is irregular. He also has a history of coronary artery disease.
- A: He’s pale, slightly short of breath, and says the pain started after walking to the bathroom.
- R: I recommend notifying the on-call physician, ordering a formal chest X-ray and EKG, and continuing to monitor his vital signs closely.
Example №2: Pediatric Patient with High Fever
- S: Hi, this is Emily from Pediatrics. I’m calling about Mia, a 4-year-old in room 205, who has spiked a fever of 103.1°F.
- B: She was admitted earlier today with abdominal pain and vomiting. Her admitting diagnosis was gastroenteritis. She's had one round of IV fluids.
- A: She's more lethargic than earlier, and her heart rate is elevated at 142 bpm. Her respiratory rate is up slightly, too.
- R: I recommend a repeat set of labs, possibly a blood culture, and notifying the pediatric team. She may also need another fluid bolus if her condition doesn’t improve.
Example №3: Post-Op Patient with Drop in Blood Pressure
- S: This is Kevin, RN on Surgical Step-Down. I’m calling about Ms. Lin, post-op day one from an abdominal hysterectomy. Her blood pressure has dropped to 82/50.
- B: She was stable earlier, with BP around 118/76. She’s been tolerating oral fluids and was walking earlier today. Her hemoglobin was borderline pre-op.
- A: She’s dizzy when standing, pale, and says she feels “weird.” Her pulse is now 112 and irregular.
- R: I suggest labs to check her hemoglobin, possibly a stat H&H, and that we notify the surgical resident. We may need to hold oral fluids and go back to IV.
Example №4: Elderly Patient with Confusion and Agitation
- S: This is Laura, night shift RN on Geriatrics. I’m calling about Mr. Patel in room 108. He’s become increasingly confused and agitated over the last two hours.
- B: He was admitted with a urinary tract infection and has a history of early dementia. His vital signs have been stable, and he was oriented earlier this evening.
- A: He’s now disoriented, pulling at his IV, and trying to get out of bed. No fever, but his pulse is elevated.
- R: I recommend checking a repeat urinalysis, possibly ordering a CT if the behavior worsens, and asking the physician about a one-time low-dose sedative if needed.
Example №5: Respiratory Distress in a Patient with Pulmonary Embolism
- S: Hi, this is James from the ICU. I’m calling about Ms. Rivera in room 402. She’s showing signs of respiratory distress.
- B: She was admitted yesterday with a confirmed pulmonary embolism. She’s been on anticoagulants and breathing treatments. Her vitals have been stable until now.
- A: Her respiratory rate is up to 32%, oxygen saturation dropped to 88% on 4L nasal cannula, and she’s reporting sharp chest pain with inspiration.
- R: I recommend increasing her oxygen support, ordering a formal chest CT, and notifying the pulmonary team immediately. This may require rapid response if she worsens.
Final Thoughts
Examples of SBAR in nursing give you a chance to communicate information in a well-organized manner. When you’re in the middle of a shift, speaking up can take a lot of effort if you're not following a clear structure. SBAR helps you say what matters without overexplaining.
And if you're dealing with nursing assignments while taking long shifts, our professional essay writers can help with that, too. We'll take care of your academic responsibilities, so you can focus on getting practical experience. Strong collaboration also matters in clinical settings - check out these examples of effective team dynamics to see how communication and teamwork make a real difference.
FAQs
What Does SBAR Stand for in Nursing?
SBAR is an acronym for Situation, Background, Assessment, and Recommendation.
What Is the SBAR Format in Nursing?
It’s a four-part way to organize patient info so it's easy to understand and act on.
What Is SBAR Used For?
Nurses use it to share patient updates quickly and clearly with HCPs or other nurses.
What is the importance of SBAR in nursing during busy shifts?
SBAR helps nurses share patient information, even when the unit feels loud or rushed. The structure keeps the update focused. It highlights the situation, background, assessment, and the action needed next. This approach reduces misunderstandings and supports safer decision-making during handoffs or urgent consults.
How to give SBAR nursing report that feels organized?
Start with the situation in a single sentence, then follow with brief background notes. Add your clinical assessment and finish with the action you recommend. Many nurses jot down short cues before speaking so the report flows smoothly.
Sources
Agency for Healthcare Research and Quality. (n.d.). SBAR technique for communication: A situational briefing model. AHRQ. https://www.ahrq.gov/teamstepps-program/curriculum/communication/tools/sbar.html
Müller, M., Jürgens, J., Redaèlli, M., Klingberg, K., Hautz, W. E., & Stock, S. (2018). Impact of the communication and patient hand-off tool SBAR on patient safety: A systematic review. BMJ Open, 8(8), e022202. https://pmc.ncbi.nlm.nih.gov/articles/PMC5123547/


